In an era where data fuels innovation, analytics capabilities have expanded exponentially across industries, revolutionizing healthcare significantly. Protected Health Information (PHI) is at the core of this transformation, offering immense potential for enhancing patient outcomes and operational efficiencies. Yet, alongside opportunities come risks—especially concerning privacy, compliance, and ethical considerations. Organizations today stand at the crossroads of leveraging PHI for analytical prowess and safeguarding sensitive information to comply with stringent regulations like HIPAA. Mastering the art and science of PHI de-identification isn’t just beneficial—it’s essential for any innovative healthcare analytics initiative seeking robust, secure, and compliant data infrastructures.
Understanding the Importance of PHI De-identification
Data-driven decision-making has become a mainstay in healthcare, providing executives and analysts with the insights required to optimize patient care, lower operational costs, and deliver targeted treatments. However, the sensitive nature of Protected Health Information presents privacy and compliance risks when exposed or mishandled. De-identification techniques fundamentally alter datasets, removing details that directly or indirectly identify individuals, rendering data anonymous and suitable for analytical exploration without breaching privacy standards such as those mandated by HIPAA.
A robust approach to PHI de-identification enables healthcare organizations to effectively share sensitive data internally and externally, driving collaboration with research institutions, academic partners, and clinical trial teams. Further, properly anonymizing data safeguards the organization against reputational damage, regulatory fines, and legal repercussions, which can often be expensive and time-consuming. Striking a balance between transparency in analytics and stringent privacy controls positions organizations for enhanced innovation, allowing leadership teams to pursue advanced analytics initiatives such as accurate demand prediction with confidence in compliance and ethical standards.
Exploring Techniques for De-identifying Protected Health Information
Data Masking & Redaction
Data masking involves replacing sensitive identifier fields, such as patient names or Social Security numbers, with fictitious yet realistic-looking values. This method ensures that the data maintains its utility for analysis while completely removing identifiable references. Similarly, redaction stands as another method, directly removing or substituting sensitive mentions within free-text fields, notes, clinical observations, or medical histories.
Automated masking and redaction solutions streamline the de-identification process, leveraging software to quickly and consistently preprocess large datasets without significant overhead. For instance, adopting smart masking processes enables organizations to engage consultants for advanced services like Microsoft SQL Server consulting services, effectively facilitating compliant analytics capabilities on healthcare data. Moreover, by incorporating automated masking solutions, implementation timelines reduce significantly without compromising privacy.
Pseudonymization & Tokenization Techniques
Pseudonymization involves the substitution of identifying attributes for encrypted fields or reference keys, preserving data integrity yet significantly enhancing patient anonymity. This methodology retains a robust link between datasets to allow precise analytics while ensuring individuals remain anonymous externally. Tokenization, similarly, substitutes sensitive data elements with non-sensitive identifiers (tokens) securely leveraging encryption frameworks or dedicated token vaults that maintain the ability to reverse mapping when necessary.
When organizations look towards advanced integration frameworks, employing tokenization and pseudonymization within innovative methods such as asynchronous ETL choreography ensures heightened security practices and better support for large-scale, real-time analytics implementations. These techniques enable unmatched flexibility and agility, empowering healthcare data-driven decision-making for strategic leadership positions and clinical research stakeholders.
Statistical Data Aggregation and Generalization
Another impactful de-identification approach focuses on aggregation and generalization methods—grouping individual records into broader data categories reduces granularity and anonymizes patient identities inherently. For instance, shifting individual age entries into broader age bands or geographic precise zip codes into regional aggregates considerably reduces identifiability risks while still preserving analytical value.
Aggregation methods prove particularly beneficial in visualizing healthcare data trends securely and meaningfully. Sophisticated visualization techniques such as violin plot implementations or highlighted metrics enabled via effective color used in data visualization amplify coherent narrative storytelling despite aggregated data. Integrating these statistical aggregation methods delivers unmatched data visibility for healthcare-driven analytics initiatives while staying confidently compliant with regulatory boundaries surrounding PHI.
Implementing Compliant, Scalable, and Sustainable De-identification Procedures
Technological Automation and Transparent Data Governance
Effective long-term de-identification practices require a combination of technological automation and governance policies, facilitating ongoing compliance. Organizations should establish clear data governance frameworks that outline roles, responsibilities, and procedures for PHI treatment, anonymization, access, and monitoring. Pairing this robust governance with technological solutions—such as metadata management, automated workflows, and monitoring assessments—helps organizations streamline the de-identification process sustainably, consistently applying protocols across distributed IT ecosystems.
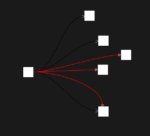
Transparent data governance is also critical in maintaining stakeholder trust & compliance transparency. Employing advanced methodologies like explainable computation graphs for transparent data transformations ensures stakeholders understand precisely how data is altered, building confidence for internal decision-makers, external auditors, and patients themselves. By harmonizing technological automation and informed governance, healthcare organizations enhance agility in responsibly leveraging sensitive datasets for analytical innovation.
Considering Compliance Risks and Cost Prioritization
Investing in robust, scalable PHI de-identification techniques is essential in managing long-term compliance-driven costs. Failing to adequately anonymize data or neglecting evolving compliance standards can attract severe regulatory fines or litigation expenses. As healthcare analytics scales through cloud-based SaaS providers, evolving subscription frameworks can quickly contribute additional costs, further elevating financial risks. Companies must carefully assess partnerships, subscription models, and long-term operational costs, recognizing that “the SaaS you picked yesterday will be more expensive tomorrow.”
Decision-makers must carefully weigh technology implementations, ensuring that de-identification techniques balance security, accuracy, usability, and cost considerations. Working strategically within frameworks that include accurate cost estimation, transparent data governance, and technological automation ensures scalability, flexibility in analytics, and a confident alignment with emerging privacy and compliance requirements.
Enhancing Analytics Insights With Anonymized PHI Data
De-identification methods augment analytical possibilities in healthcare. Properly anonymized, PHI data remains immensely valuable, supporting critical applications such as predictive analytics, disease research, health equity assessment, clinical quality improvements, and business intelligence. Through advanced approaches like embedding statistical context in data visualizations or creating hierarchical models via recursive data processing, influential analytical insights are unlocked, benefiting care outcomes, optimizing resources, reducing costs, and enhancing healthcare services delivery extensively.
Furthermore, iterative analytical improvement practices support healthcare dashboard performance through strategic performance tuning for data visualization dashboards—delivering insights faster, securely, and with greater accuracy. Empowered by compliant, de-identified data, healthcare organizations harness transformative analytics capabilities, positively impacting patient care, population health management, and healthcare innovation, firmly placing organizations at the forefront of responsible data-driven healthcare.
Conclusion
De-identification techniques for Protected Health Information are mandatory means for healthcare institutions seeking robust analytical capabilities and regulatory compliance. By employing strategic masking, redaction, tokenization, and aggregation methods coupled with transparent governance, technology automation, and scalable analytics infrastructure, organizations elevate data privacy, enrich analytics insights, and confidently meet regulatory obligations—charting the path to innovative, data-supported healthcare operations.
Thank you for your support, follow DEV3LOPCOM, LLC on LinkedIn and YouTube.